After Your Los Angeles Medicare Fraud Arrest: Are You on the Flywheel or the “Doom Loop”?
Ever since authorities began investigating you for Medicare fraud in Southern California, you’ve been overwhelmed, uncertain, and scared for your reputation and your family’s future. 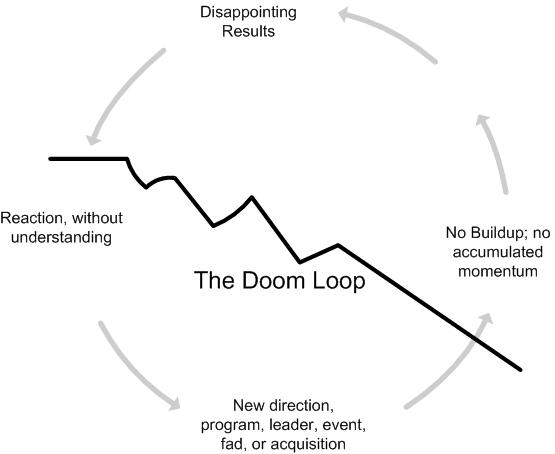
Life, it seems, has taken an unexpected and decidedly unwelcome turn.
Given your hectic state of affairs, you might be laboring under some false assumptions about the trajectory of your life and welfare. In other words, all the legal chaos may bias you into believing that things are “getting worse” or “will get worse” for you.
 Los Angeles Criminal Defense Attorney Blog
Los Angeles Criminal Defense Attorney Blog